AHA News: Stroke Rehab Improves Recovery. So Why Aren't Hispanic Survivors Getting Enough of It?
By American Heart Association News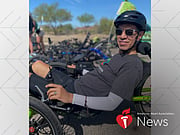
MONDAY, May 22, 2023 (American Heart Association News) -- Joe Granados was slumped in a chair when his wife – alerted by their children – came to check on him. He didn't seem like himself.
Alba Patricia Granados, a nurse, quickly realized her husband was having a stroke. "He couldn't speak, and he couldn't move the right side of his body," she said.
Joe had experienced similar symptoms earlier that morning but had recovered by the time he told his wife. Neither was too concerned because eight months earlier – the first time he had trouble walking and felt weakness in his right arm – doctors had attributed the symptoms to a possible migraine. After undergoing medical tests, he left the hospital in July 2021 with a clean bill of health.
But on that day in March 2022, doctors at a hospital near the family's home in Tucson, Arizona, said Joe was having a stroke. Complications emerged during surgery to remove a clot from a large vessel in his brain, but Joe survived. He was less than a month from his 52nd birthday.
After a couple of weeks in the hospital and six weeks at an inpatient rehabilitation center for speech, physical and occupational therapy, Joe returned home. He still attends outpatient rehab for three hours each week.
While Joe has regained partial movement and limited speech, Alba describes his post-stroke recovery as mixed. "With a cane or a walker with a base, he can walk short distances from one end of the house to the other, but he might have to take breaks," she said. "He still needs some help getting dressed, but most of his personal hygiene he can do, and he can eat by himself."
Joe's experience is not unusual. Stroke is a leading cause of disability in the United States, and some studies suggest Hispanic stroke survivors like Joe may have worse outcomes and greater disability than their white peers.
A potential reason may be disparities in stroke rehabilitation, where survivors relearn basic skills such as eating, talking and walking. A nationwide study published in the journal Stroke this year found Hispanic participants received disproportionately lower amounts of physical therapy and occupational therapy during the first year of stroke recovery.
Other research published in Ethnicity & Disease in 2019 found that Hispanic stroke survivors at an inpatient rehab facility in Southern California were more likely than white survivors to be discharged home. The researchers said that may reflect an implicit bias within health care systems to send Hispanic survivors home rather than to a skilled nursing facility or other setting with stroke recovery services. Or, they said, it may reflect the value of "familismo" in the Hispanic culture that includes commitment to caring for family.
Dr. Jose Rafael Romero, a neurologist at Boston Medical Center, said the type of rehabilitation that patients receive in the immediate weeks following a stroke is a key factor in their recovery.
"While several factors affect stroke recovery, most of the recovery happens in the first two to three months after the event, while slower improvements can be noted over the long term," said Romero, who also is an associate professor of neurology at Boston University. "For example, the size of stroke is an important factor. If a person has a large stroke with major deficits like paralysis on one side, inability to speak and loss of vision in one side, recovery is typically very slow and may not be complete."
He said that although doctors can estimate within the first few days whether someone is likely to have "major residual deficits," it is difficult to predict the final degree of recovery.
Inpatient therapy is the most intensive form of rehabilitation, and research shows it can produce better outcomes.
But preliminary research presented in February at the International Stroke Conference found Mexican American stroke survivors in South Texas were more likely than their white peers to use outpatient and home health rehabilitation – and they had worse functional outcomes three months after their stroke. The study is ongoing with plans to publish a comprehensive study within two years, lead researcher Lynda Lisabeth said.
"We're hoping to look at whether or not there are ethnic differences in the use of inpatient rehabilitation in particular, and then look at whether or not that first initial post-acute rehabilitation setting influences the ethnic differences in stroke outcomes that we've observed," said Lisabeth, a professor of epidemiology at the University of Michigan in Ann Arbor.
The goal of the study, she said, is to "understand factors that may facilitate or serve as barriers to use of inpatient rehabilitation." That would allow stroke care teams "to optimize post-acute care both from an economic standpoint, but also from a sociocultural perspective."
As research continues, Romero said improving stroke recovery for Hispanic people will require making it easier for them to access health care, insurance and health care professionals who can offer personalized, culturally tailored care – including Spanish interpreters when needed.
"Even when they have insurance, factors like language barriers are important ones to consider," he said. "If there are no therapists that can understand the patients or they don't use resources to communicate, like translators or interpreters, the assessments done to check the potential for recovery may be limited. And when they are undergoing therapy, the patients may be less likely to understand what they're supposed to do and to do it properly, thus affecting potential for recovery."
Back in Tucson, Alba said Joe, who is fluent in English and Spanish, usually spoke English before his stroke. But when he started speaking again after his stroke, he began to use more Spanish words.
"I don't think they could tap too much into that during rehab because most speech pathologists don't speak Spanish," Alba said. "So, I wonder what happens to people who are Spanish-speaking only."
Joe's speech has improved during the past year, but he can't yet hold a conversation. Still, Alba is hopeful he will continue to make progress in speaking and other basic skills with help from weekly outpatient therapy, as well as group speech therapy through the local nonprofit Friends of Aphasia – and a new favorite activity.
"He recently started riding recumbent trikes, and it's like the whole world opened up to him," she said.
American Heart Association News covers heart and brain health. Not all views expressed in this story reflect the official position of the American Heart Association. Copyright is owned or held by the American Heart Association, Inc., and all rights are reserved.
By Lourdes Medrano, American Heart Association News

The news stories provided in Health News and our Health-E News Newsletter are a service of the nationally syndicated HealthDay® news and information company. Stories refer to national trends and breaking health news, and are not necessarily indicative of or always supported by our facility and providers. This information is provided for informational and educational purposes only, and is not intended to be a substitute for medical advice, diagnosis, or treatment.

